New Hope for Cleft Palate
 The results of an innovative new procedure were recently revealed in the Journal of Craniofacial Surgery. Five years in the making, the procedure was performed on a then-newborn baby (now age 5) who was diagnosed with the condition cleft palate in the womb. Cleft palate is a congenital condition wherein the roof of the mouth (the palate) is split (cleft) due to the palatal shelves failing to properly close during the embryonic stage.
The results of an innovative new procedure were recently revealed in the Journal of Craniofacial Surgery. Five years in the making, the procedure was performed on a then-newborn baby (now age 5) who was diagnosed with the condition cleft palate in the womb. Cleft palate is a congenital condition wherein the roof of the mouth (the palate) is split (cleft) due to the palatal shelves failing to properly close during the embryonic stage.
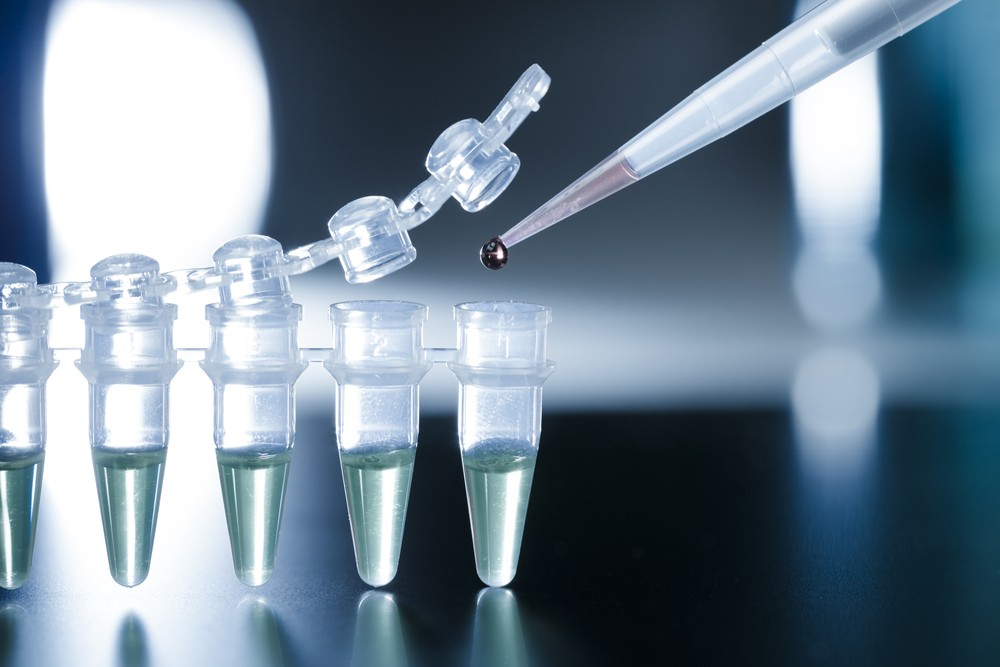
Researchers at Hospital de San Jose in Bogota, Colombia, took embryonic stem cells from the subject’s umbilical cord at birth and froze them. After several months of a procedure called nasoalveolar shaping, the stem cells were thawed and used in a procedure called gingivoperiostioplasty. Using a biomaterial known as gelfoam, the cells were inserted into the soft tissue in the upper jaw, helping to close the cleft in the palate during a cheiloplasty procedure.
Dr. Gary Lederman of Bellmore, New York, says procedures such as this can be hugely beneficial to children born with cleft palate, but also could someday be beneficial to patients suffering from other facial conditions such as temporomandibular joint disorder.
"The success of this surgery is wonderful news and certainly something to celebrate," says Lederman. "Hopefully the success of the stem cells helping to generate bone will be able to be parlayed into other types of surgery, such as procedures to correct bone deterioration from TMJ disorder."
For now, researchers are celebrating a win five years after the birth of the first recipient of the cleft palate surgery - and rightfully so.



